Weight-Loss Surgery
Sleeve gastrectomy
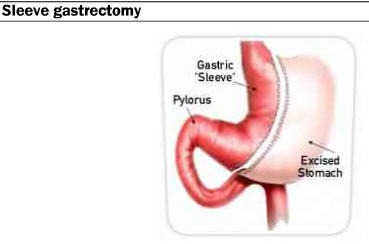
Sleeve gastrectomy procedure (mostly performed laparoscopically) removes approximately 70% – 80% of the stomach, leaving a sleeve in place. The big benefit of this approach is that even though the volume is reduced, most of the gastric nerves are left intact and the function of the stomach is not impacted. Furthermore, it is believed that with the removal of the fundus (located along the larger curve of the stomach), there are positive effects to the gastrointestinal hormones releases, such as ghrelin, which can reduce hunger.
Biliopancreatic diversion (BPD): aggressive removal, aggressive results
These procedures crate the most extreme results in bariatric surgery. In this procedure approximately 70% of the stomach is actually removed. Biliopancreatic diversions are similar to gastric bypass in that its purpose is to both restrict the volume that is able to be digested and also to create malabsorption.
1. The stomach is horizontally cut to create a six ounce pouch with the excess portion of the stomach completely removed from the body.
2. The modified stomach is connected directly to a shortened small intestine, bypassing the duodenum and jejunum, approximately 50-100 cm from the colon allowing for malabsorption.
3. Digestive enzymes are passed from the gall bladder and pancreas through the bypassed portion of the small intestine which is reconnected to the ileum portion of the modified small intestine.
4. When this is done with a duodenal switch, the stomach is cut vertically forming a tube shaped stomach which empties into a shortened duodenum. Again, the food has a shortened channel where it can be mixed with bile and pancreatic juices to be digested; however, the duodenal switch allows for improved capture of iron and calcium.
Compared to conventional gastric bypass, the %EWL (excess weight loss) outcomes are often superior with the biliopancreatic diversion with a duodenal switch, and patients are often more satisfied with the new lifestyle because they can consume a larger volume (compared with bypass) of high calorie food without full absorption. Data suggests patients receiving biliopancreatic diversion achieve %EWL of 70% with weight loss persisting through long term (up to 18 years) follow-up.
However, the intensive malabsorptive component of these procedures is so significant that patients are required to take vitamins and minerals supplements to prevent malnourishment. The adverse effect of the duodenal switch is dumping syndrome, where food is passed too quickly into the small intestine without being digested. Dumping is associated with nausea, bloating, and rapid heart rate after consumption of fine sugars. These risks, along with the high degree of technical difficulty performing the procedure, makes it a rarely utilized therapy.

