Clinical Complications: How FAT Destroys The Body From the Inside Out
There is little mystery as to how a person accumulates excessive amounts of fat, and in many cases, it is controllable and preventable. Weight gain is a simple imbalance of caloric intake being higher than caloric expenditure (we eat too much and move too little). So what is wrong with being big? While the debate goes on as to whether or not obesity is an actual “disease” itself, there is no debate as to the implications on patients’ overall health.
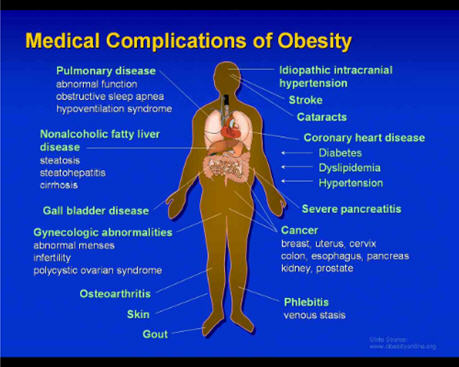
The long list of health consequences associated with being obese is the result of two independent factors: 1) the increase in the mass of the adipose tissue or number of fat cells, or 2) the secretion of pathogenic products or metabolic effects from the enlargement of fat cells. The figure below highlights the various and numerous risks associated with obesity.
Problems linked to the increased mass of fat cells
Obstructive sleep apnea: the fat can literally choke you
The respiratory complications clinically linked to excess abdominal and upper body fat focus on sleep disorders. Air passageways and lungs become constricted by excess adipose tissue temporarily blocking the passage of air, making it difficult to breathe. Obstructive sleep apnea (OSA) is defined as episodes of cessation in breathing for at least 10 seconds during sleep.
Typically the symptoms are vague, such as fatigue, irritability, snoring, and morning headache. The lack of REM (rapid eye movement) sleep can lead to emotional and behavioral problems, including overeating which exacerbates the problem.
Complications due to OSA mostly lie within the cardiovascular system. When the bloodstream is deprived of oxygen (oxygen desaturation), patients will typical become hypertensive. This low-oxygen, high-blood-pressure state can bring on cardiac events, especially in cases where there is preexisting heart disease.
The first line of defense that physicians prescribe to these patients is lifestyle changes:
• Weight loss program to relieve constriction of the throat. Medical and surgical studies have shown that as little as a 10% decrease in weight is associated with a 50% reduction in sleep apnea severity. Even very moderate weight reduction in obese patients can lead to significant improvement in oxygenation and blood pressure.
• Avoid consuming alcohol, sleeping pills, and any medication that will promote the relaxation of the muscles in the back of the throat.
• Sleeping on your side or stomach to prevent the tongue and soft palate form resting against the back of the throat, blocking the airway.
• Use of saline nasal spray, decongestants, or antihistamines to keep nasal passages open at night.
Moderate to severe cases are addressed with non-surgical devices:
• Oral devices can be prescribed and work by bringing the jaw forward, helping keep the throat opening and prevent obstruction. These products are easy to use and can be purchased from dentists.
• Supplemental oxygen can also be supplied ruing sleep. Simply increasing the oxygen content in the blood can relieve many of the OSA symptoms.
• Continuous positive airway pressure (CPAP) has patients wear a face mask that applies constant positive air pressure during sleep. These devices keep the upper air passages open, preventing snoring and apnea.
• Bilevel positive airway pressure (BiPAP) is similar to CPAP but increases pressure during inhalation and decreases during exhalation.
For extreme cases, a surgical procedure is the only sure fix:
• The Pillar Procedure by Restore Medical places polyester implants into the soft palate. These implants add support to and stiffen the soft palate, helping reduce obstruction in the upper airway.
• Uvulopalatopharyngoplasty (UPPP) is a procedure that removes obstructive tissue from the rear of the mouth and back of the throat (tonsils and adenoids).
• The maxillomandibular advancement procedure brings the jaw forward, away form the face. The effect is similar to the oral device.

